Dr Umanath Nayak
Dr Umanath Nayak, Fellow of the University of California, Davis (U.S.A.) is a Best Head & Neck cancer specialist with over 25 years of expertise in managing Head & Neck cancer and related tumors and conditions. He is Chief Consultant in Head & Neck Surgery and Oncology at the Apollo Cancer Institute, Hyderabad and Co-ordinator of the Head & Neck Fellowship program.
Services
- Salivary Glands
- Oral cancer
- Thyroid Nodule
- Throat Cancer
The salivary glands:
- Parotid gland – Largest and most important. Located one on each side of the cheek
- Submandibular gland – one on each side under the jaw
- Sublingual gland – in the midline under the chin
- Numerous tiny glands spread all over the inner lining of the air and food passages of the Head & Neck.
Function:
Production of saliva to aid in digestion and maintain the normal lubrication of the oral cavity.

Conditions affecting the salivary glands that may require surgery:
- Submandibular salivary gland may be affected by repeated infection (caused by stones in their duct).
- Tumors – usually benign, occasionally malignant

- Pleomorphic adenoma: Most common. Though benign it requires surgical removal in view of its propensity for growth and rare instances of malignant conversion.
- Malignant tumours – Less common, more dangerous Muco-epidermoid carcinoma, Adenoid cystic ca and others
The challenge in any Parotid surgery is identification and preservation of the facial nerve and its branches. The facial nerve is responsible for the normal movements and expression of the face and damage to its branches affect these movements.
Types of surgery for tumors of Parotid gland:
- Superficial Parotidectomy: Tumor is removed along with a margin of normal parotid tissue.
- Total conservative Parotidectomy: Removal of the entire gland preserving the facial nerve.
- Total radical parotidectomy : Removal of entire gland along with the nerve. Generally recommended for aggressive cancers which may already have affected the nerve and caused paralysis.
Note:
- In certain cancers lymph nodes in the neck may also be removed during the Parotidectomy operation.
- Following surgery many patients with cancer are advised to take post-operative radiation therapy to reduce the risks of relapse.
In general low-grade cancers have an excellent chance of cure with proper surgery. High grade cancers may not do as well, but surgery followed by post-operative radiotherapy can still offer good control for many years.
For more information on Salivary gland tumors you may contact at drumanathknayak@gmail.com or Ms. Archana on 91-9391369493
Oral cancer
Oral (mouth) cancer is a very common cancer in our country. This cancer is associated with the rampant habit of chewing tobacco in different forms as well as smoking and drinking alcohol. Ignorance, poor nutrition and low socio-economic conditions result in a majority of these cancers being detected at an advanced stage when treatment (mainly surgery) is challenging and cure rates are low. Awareness and regular screening of the population at risk (tobacco users) can identify these cancers at an early stage when surgery can result in a high rate of cure with minimal morbidity and better functional outcomes. Screening can also aid in identifying pre-cancerous conditions and instituting measures to reverse them before they can progress to frank cancer. Along with the examination and evaluation, education and counselling to break the habit of tobacco usage also forms an important part of the screening program.
Warning signs:
- An ulcer or sore in the mouth or lips which persists beyond 3 weeks
- Swelling or growth on the tongue which may or may not be associated with pain and/or difficulty in chewing or swallowing
- Persisting ulcer or swelling over the jaw associated with loosening of teeth
- Blood in sputum or saliva which persists despite the treatment of any associated gum infection
- A painless, progressive lump in the neck
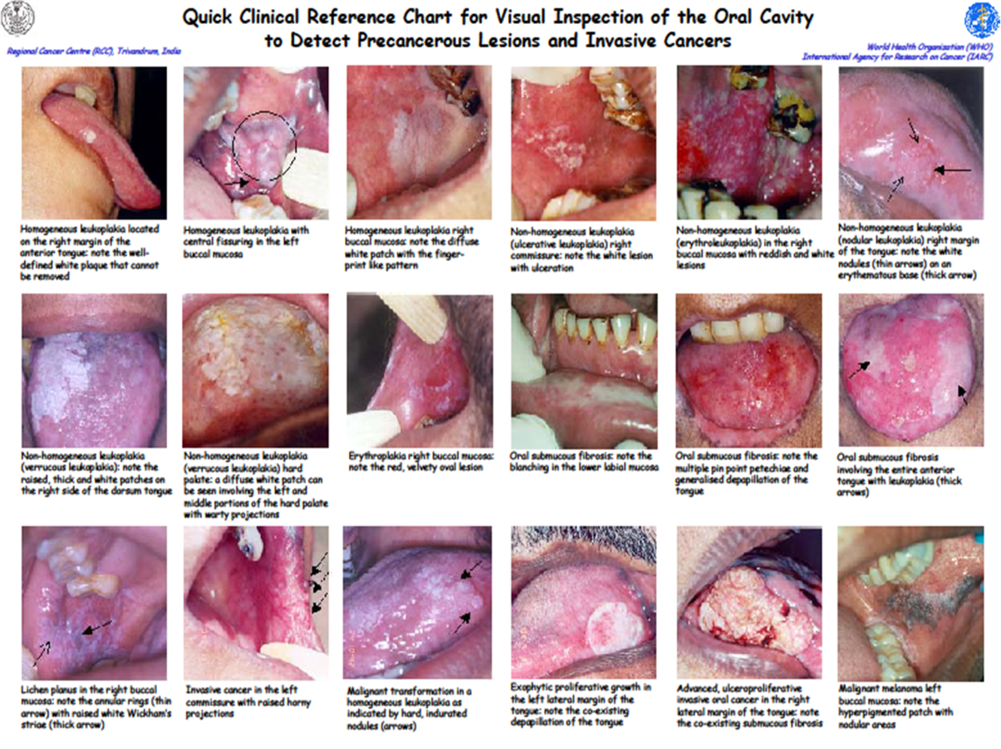
Pre-cancerous conditions associated with chronic tobacco use:
- Leukoplakia: A white patch in the mouth which does not go away when rubbed
- Erythroplakia: A red velvety patch which may be associated with pain or burning while eating
- Oral submucous fibrosis: Diffuse blanching/pallor and thickening of the mucosa (lining) of the mouth associated with intolerance to spicy food, loss of elasticity of the cheeks and restricted mouth opening.
Articles
Treatment:
Early stages of oral cancer (1 and 2) are highly curable by surgery. The cancer is removed along with a margin of normal tissue around it. Sometimes a margin of the jaw bone and/or lymph glands in the neck may also need to be removed depending on the location of the cancer. In early cancer surgery results in minimal morbidity and overall functional and cosmetic outcomes are excellent. Following surgery the excised specimen is sent for histopathological examination (detailed biopsy) and if there are adverse features such as involvement of the lymph glands by cancer cells, radiation may be given post-operatively after 4-6 weeks to reduce the risks of a relapse.On the other hand, surgery for advanced stages (3 and 4) is more difficult and challenging, and overall cures may also be less. Surgical removal of the cancer can also result in functional and cosmetic disturbances, but with the latest available reconstructive methods the outcomes are acceptable. Almost all of these patients require post-operative radiotherapy and in certain cases chemotherapy.
For more information about oral cancer you may contact at
drumanathknayak@gmail.com or Ms. Archana on 91-9391369493
Thyroid nodule
Thyroid nodule (a lump or swelling in the thyroid gland) is a common occurrence and is seen in about 10-12% of the normal population (Figure 1). The vast majority of these nodules are benign and not dangerous and unless progressing or causing symptoms, they can be left alone and not operated upon. However, a small percentage (about 5%) of these nodules can be cancerous (malignant) and surgery becomes mandatory to remove the diseased gland. Quite often, the challenge is to differentiate between benign and cancerous nodules. Clinical examination and investigations such as ultrasound and needle aspiration (FNAC) can often help in determining the risks of cancer and nodules that have a higher chance of being malignant are usually operated upon. Sometimes the surgeon may order an intra-operative pathological examination (frozen section) to determine if the nodule is malignant or not.


Surgery (thyroidectomy):
In experienced hands thyroidectomy is a safe operation and the cosmetic outcomes are very satisfactory with a minimal scar that fades with time (figs 2-4). In recent times, the option of remote access surgery (surgery from a distant site such as the armpit or inner aspect of the lip using specialized techniques) can be offered if the patient is desirous of avoiding a visible scar in the neck. During surgery if the nodule is restricted only to one side and is not malignant, then only one half of the gland is removed (hemi-thyroidectomy) and if the entire gland has nodules or if the nodule is malignant, then total removal of the thyroid gland (total thyroidectomy) is the recommended treatment. Total thyroidectomy is a safe operation and the patient has to take a thyroid hormone replacement medication (thyroxine) throughout life.
Thyroid cancer:
Cancer of the thyroid gland is an uncommon cancer and accounts for just about 1%–1.5% of all cancers. Though in India no clear data is available, in the USA, the incidence of this cancer has shown a 2.4-fold increase in the last three decades (from 3.6 per 100,000 of the population in 1973 to 8.7 per 100,000 in 2004). This is believed to be due more to better diagnostic facilities such as ultrasound, which can pick up thyroid nodules much earlier, rather than any true increase in the incidence of the cancer. Exposure to ionizing radiation is one of the known risk factors for the development of thyroid cancer and the cancer often develops decades after the exposure has occurred.
The regular type of thyroid cancer (commonly referred to as well-differentiated thyroid cancer) is one of the most curable cancers known and provided that adequate surgery is performed, most (95%) of the younger patients (below 45 years of age) with this cancer live their normal lifespan. Surprisingly, older patients with this cancer do not do so well. This is the only cancer in which the age of the patient is a very important factor determining the aggressiveness of the cancer and survival. One variant of thyroid cancer, the medullary carcinoma of thyroid or MCT, has a genetic basis and a sub-group of patients with this condition have been found to carry an abnormal gene, the RET proto-oncogene. The identification of this gene in subjects at risk (first-degree relatives of those with familial MCT) can predict with 100% accuracy the future development of thyroid cancer.
Treatment of thyroid cancer:
The recommended treatment for thyroid cancer is surgery – Total thyroidectomy. If surrounding lymph nodes are involved then a neck dissection (removal of the lymph glands along with surrounding fat) is also done. Post-surgery a certain section of patients (older patients, those with large tumors, lymph node spread or spread into other parts of the body) are treated with high-dose radio-iodine therapy, which is administered a month after surgery. This treatment is routinely given post-operatively to all high-risk thyroid cancer patients to eradicate any cancer which may not have been addressed by surgery or to destroy microscopic cancer that may be lurking unseen in any part of the body. Thyroid tissue (cancerous or otherwise) concentrates iodine and the radioactivity in the administered iodine destroys it. Following this treatment, patients are kept isolated in a special room for 24-48 hours, since the radioactivity could be harmful to others around them.
Following the completion of treatment patients are put on thyroid replacement hormone (thyroxine) the dose of which is higher than when used as replacement therapy in benign conditionsn and are are regularly followed up with serial serum thyroglobulin estimations.
If you have a thyroid nodule and need more information you may contact at
drumanathknayak@gmail.com or Ms. Archana on 91-9391369493
The term ‘throat cancer’ is commonly used for cancers involving the larynx (voice box) and the hypopharynx (upper part of food passage). Cancer of the throat is common in our country, accounting for over 12% of all cancers. These cancers are generally caused by the habit of smoking or chewing tobacco and may be curable if detected early.
Patients initially present with either change in voice (larynx) or pain during swallowing (hypopharynx) but as the disease advances they can develop breathing difficulty, obstruction to swallowing or blood in their sputum. In some cases they may only present with a lump in the neck and the primary cancer may be silent.
Treatment:
A. Cancer of Larynx:
- Early cancer of the larynx (first and second stages) is treated either by radiation therapy or by a surgical procedure called trans-oral laser surgery, which involves cutting out the cancer with a laser beam directed through an endoscope.
- In moderately advanced cancer of the larynx (third stage) although surgery in the form of total laryngectomy results in a higher percentage of cure than other forms of treatment, considering the psychological impact of the loss of the normal voice and the presence of a permanent stoma, a non-surgical option—chemoradiation (radiation therapy along with chemotherapy)—is initially recommended to preserve the larynx. If this treatment fails, the option of surgery is then considered.
- In advanced stages (fourth stage), cancer of the larynx is still curable, though it may require a total laryngectomy (a surgical procedure involving the removal of the entire voice box). Following surgery, radiation with or without chemotherapy is generally recommended 4-6 weeks later to further consolidate the results of treatment.
A. Cancer of Hypopharynx:
Treatment policy is similar to that of cancer of larynx, but overall results of treatment and cure rates are not as good. Early stage disease is treated by radiation therapy and more advanced stages by surgery (total laryngectomy and pharyngectomy) and post-operative radiotherapy. Often the pharynx (food passage) may require reconstruction using tissues from other parts of the patient’s body (skin from chest or thigh or portion of small intestine).
C.Rehabilitation:
A person who has undergone the procedure of total laryngectomy is called a Laryngectomee. Laryngectomees do not breathe through the nose or mouth, but through an opening created in the root of the neck called the ‘stoma’.


The presence of the stoma and this altered method of communication make certain lifestyle modifications mandatory for laryngectomees. In recent times development of special appliances, such as the so-called Hands-free system, can help produce voice without digital occlusion.
To help laryngectomees adjust to their new lifestyle, to enhance their social and communication skills, and to help them deal with other issues connected with their day-to-day living, many cancer centres have a self-help groups, generally referred to as a ‘laryngectomee club’, for the rehabilitation of these patients. The Laryngectomee Society of the Apollo Cancer Institutes in Hyderabad is a similar voluntary self-help rehabilitation group which works towards the physical, social, psychological and emotional rehabilitation of the laryngectomees. The Society meets on the second Saturday of every month.
For more information about throat cancer you may contact at
drumanathknayak@gmail.com or Ms. Archana on 91-9391369493
Successes and awards
PATIENTS SERVED
CERTIFICATES & AWARDS
